
If you are searching for fresh and cutting-edge skincare techniques, you have probably come across a lot of influencers touting the advantages of red light therapy. It makes sense that new mothers looking for at-home solutions to issues they frequently encounter during the postpartum period have seen it on social media.
Actress Jenna Dewan, who gave birth to her daughter Rhiannon not too long ago, posted an Instagram carousel detailing her self-care regimen for mastitis, which involves massaging her breasts with a red light therapy mask. In this piece, we go over the definition of mastitis, discuss various management techniques, and, of course, provide an answer to the question of whether red light therapy is appropriate for treating mastitis.
Disclaimer
The language used reflects the terms in our sources. Thus, words like ‘mom/mother’ and ‘woman’ generally refer to individuals assigned female at birth (AFAB), though mastitis can affect anyone with a female reproductive system regardless of gender identity.
What is mastitis?
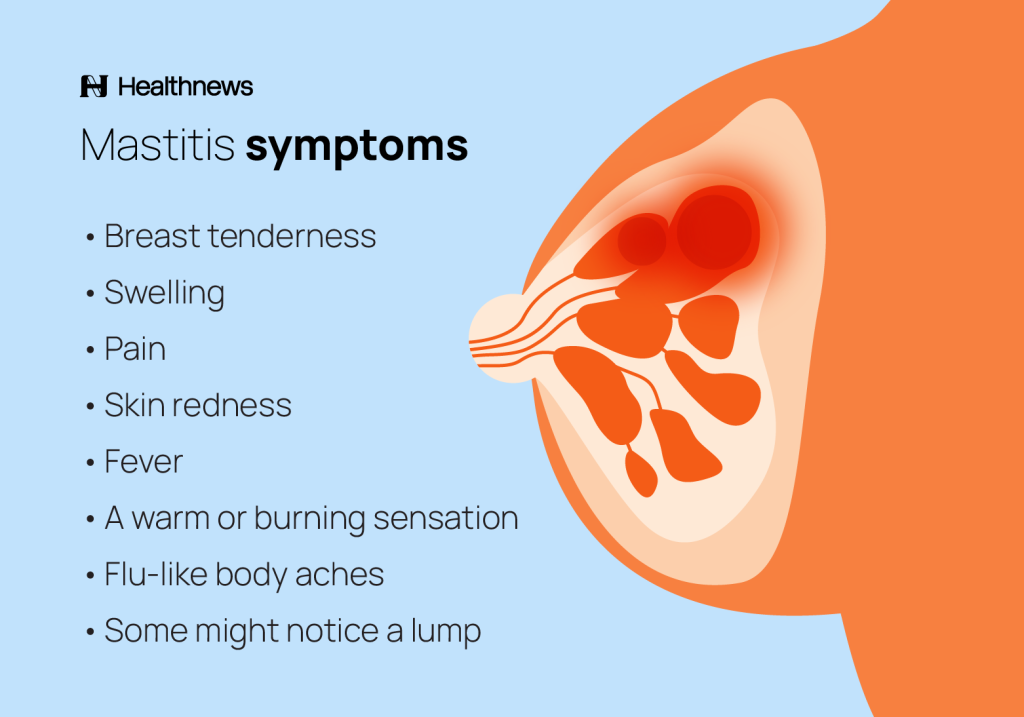
Mastitis is an inflammation of the breast tissue, and it often appears suddenly, affecting one or both breasts. It usually affects those who are nursing, but it may also affect non-nursing individuals.
Can red light therapy help with mastitis?
Currently, there is no substantial evidence to support the use of red light therapy for mastitis or any other lactation issues. Although limited research suggests that low-level laser therapy, which red light therapy falls under the umbrella of, may have an anti-inflammatory effect, it’s unknown whether it could help combat inflammation in breast tissue in particular.
To add, it is not known whether using this type of photobiomodulation is even safe in breastfeeding people, and those who use conventional lines of treatment for mastitis — antibiotics and anti-inflammatory drugs — may be at risk of increased light sensitivity.
Some very old papers of questionable quality published in the Soviet Union have described using laser sources of light (not LED devices, which most at-home red light therapy devices are) for mastitis treatment. However, evidence from studies published such a long time ago — in the 80s, to be exact — cannot be considered relevant.
A few more recent studies looked at how low-level laser therapy helped nursing women manage their nipple pain. Nevertheless, the outcomes varied, and the research did not specifically address the management of mastitis.
As a result, there is no scientific evidence to back up the use of red light therapy for mastitis.
Jenna Dewan’s mastitis routine
Jenna Dewan, the actress who posted her mastitis self-care routine on Instagram that included using a red light therapy mask on her breast, hasn’t shared her motives with her 9.5 million followers on Instagram.
The post was intended to be empowering to fellow moms — it certainly doesn’t seem like Dewan aimed to make people doubt conventional, evidence-based based-treatments of mastitis (after all, though risking a case of photosensitivity, she made it clear that she’s also using antibiotics and anti-inflammatory meds). However, the comment section of the post has become a free space for fellow Instagram users to spread fake news about mastitis treatment. To add, media sources were quick to pick up this story without pointing out the lack of substantial evidence of this treatment strategy.
What should red light therapy be used for?
It is noteworthy that there is still a dearth of research on red light therapy. Despite being a non-invasive therapy, there is no guarantee that it will be safe. We still do not know all of the possible advantages and disadvantages of red light, nor how frequently, how long, how intensely, or how far away the devices should be used.

If you’re thinking of giving red light therapy for your needs a go, first, see a healthcare professional for an adequate diagnosis and treatment and discuss whether red light is safe and potentially beneficial in your case. Then, choose a device from a reputable brand that provides extensive data on their safety standards, and make sure to thoroughly read the user manual of your device of choice.
Medically approved mastitis self-care tips
There are many self-care steps that nursing mothers can take as soon as the symptoms appear, even though red light therapy is not advised as a secure and reliable mastitis treatment option.
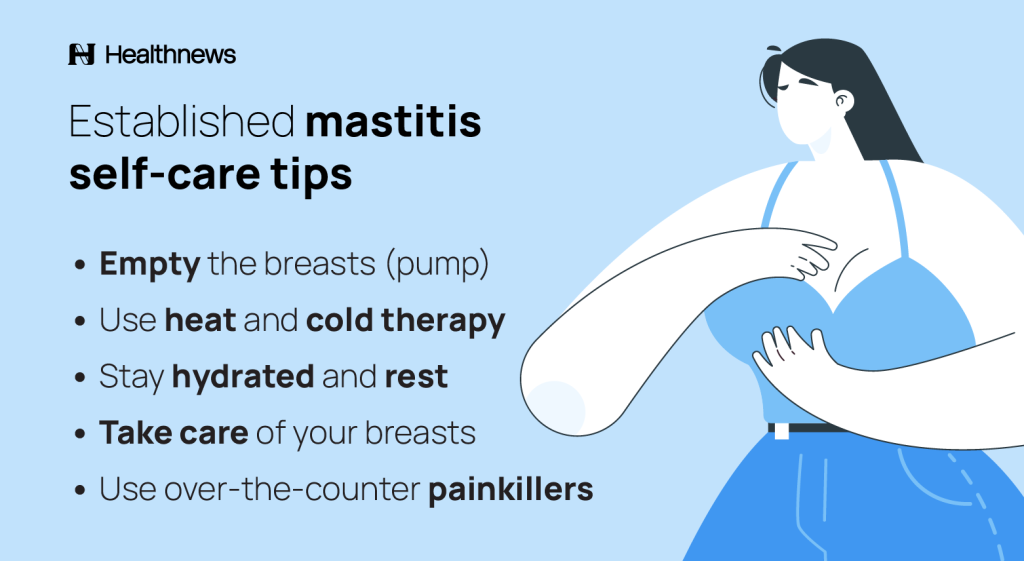
Empty the breasts
Starting from the affected side, keep up the regular breastfeeding, hand expression, and pumping to help get rid of the breast infection. The condition will deteriorate as the milk accumulates if you cease emptying the breasts.
Breastfeeding is advised even if you are prescribed antibiotics or feel like your breasts are uncomfortable full. They are safe for your baby.
To ensure that the baby is latching on appropriately, you may wish to consult a lactation consultant. Changing positions while nursing could also be helpful.
Use heat and cold therapy
Compresses are an easy-to-use, natural treatment option for mastitis. By improving the flow, applying a warm cloth to the breast prior to emptying can help increase milk letdown. Use a cold pack after nursing or emptying the breast by hand-expressing or pumping the milk. Both pain and swelling may be lessened by cold.
Stay hydrated and rest
Even though taking care of a baby can make this undoubtedly challenging, make sure to get as much rest as you can by asking your family for assistance when needed. Keep in mind that a fever can cause dehydration, so drink lots of water.
Take care of your breasts
Wait until you are comfortable with your breast size before wearing tight bras or tops. Pick softer, more supportive bras in its place. While emptying the breast, gently massage it without exerting excessive pressure. Do not apply any ointments before seeing a doctor.
Use over-the-counter painkillers
Ibuprofen and other non-steroidal inflammatory drugs (NSAIDs) are safe to take while nursing a baby. They may help reduce pain, reduce inflammation, and ease breast tenderness. Such NSAIDs are extremely unlikely to affect your unborn child.
Mastitis and red light therapy: the takeaway
It is reasonable to conclude that red light therapy has no place in the management of mastitis based on the available scientific data. Furthermore, it is unclear if red light therapy is even safe for women who are nursing.
See your healthcare provider if using home remedies does not seem to help you feel better or if you have concerns about the health of your breasts. Antibiotics may be required on occasion.
Want to know more about mastitis? Leave your questions in the comment section below.
FAQ
Is red light therapy safe while breastfeeding?
There is not any proof that red light therapy is safe to use while nursing.
Can red light therapy be used alongside other treatments for mastitis?
See your healthcare provider if you think you may have mastitis and are thinking about experimenting with non-conservative methods of self-care. However, red light therapy is unlikely to aid in your healing process, and its safety is unknown based on current scientific knowledge.
Who should not use red light therapy?
Red light therapy may be harmful to those who are pregnant or nursing, have photosensitivities, or are taking medications that increase sensitivity to light, as there is no evidence to support a different conclusion. People who are afflicted with cancer should steer clear of red lights.
Key takeaways:
- Red light therapy has gained popularity as a self-care technique for managing musculoskeletal pain, hair loss, acne, and aging skin.
- There is currently little data to back up these red light therapy advantages.
- Actress Jenna Dewan, who gave birth to her daughter recently, disclosed that she treats her mastitis with red light therapy apps.
- Even as an adjunct therapy, red light therapy for mastitis is not an evidence-based treatment approach.
- As of right now, there is no proof that using red light therapy while nursing is safe.









Leave a Reply